How Does TMS Therapy Work?
Transcranial magnetic stimulation (TMS) therapy is an innovative, FDA-approved treatment for people living with severe, clinically diagnosed depression. This noninvasive, nonpharmaceutical therapy is highly effective and often prescribed for people who cannot take antidepressant medications and those who’ve tried medications and experienced little-to-no positive results.
Unlike depression medications — which work by inhibiting the reuptake of mood- and emotion-regulating neurotransmitters, thereby prolonging their efficacy period — TMS therapy doesn’t block neurotransmitter reuptake. Instead, the therapy uses magnetic fields to help the brain release more of the neurotransmitters involved in mood and emotional regulation.
TMS therapy may be used in conjunction with medication or other therapies.
How exactly does TMS therapy work? Read on to find out.
The Basics of TMS Therapy
TMS therapy is an in-office, outpatient treatment that typically takes place in a psychiatrist’s office or a behavioral health treatment facility. As mentioned, the therapy is non-invasive, which means it does not involve any needles, incisions, sedation, or anesthesia. There are also no oral or intravenous medications involved in transcranial magnetic stimulation therapy.
Throughout each therapy session, you’ll remain fully alert and awake and can operate a vehicle safely and return to your normal daily routine after each treatment. There are minimal side effects associated with TMS, and while treatment results do vary, most patients find they experience marked symptom improvement for approximately 12 months.
An average course of treatment takes place over a period of four to six weeks, during which patients receive TMS therapy five days per week at first and then tapering down towards the end. Each therapy session lasts approximately 20-40 minutes, depending on your unique needs and your provider’s recommendation.
How TMS Therapy Works
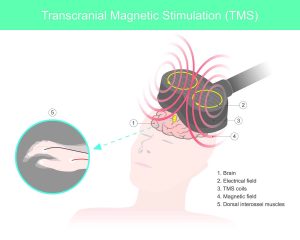
During each TMS session, your therapist will place an electromagnetic coil on your head near your brain’s prefrontal cortex. This is the area of the brain that regulates your mood. The coil produces highly concentrated pulsed magnetic fields (which are similar to those produced by an MRI machine) that turn on and off very rapidly.
Those magnetic fields travel about two to three centimeters into the brain directly below the electromagnetic treatment coil. Once inside the brain, the magnetic fields generate tiny electrical currents, which are intended to stimulate nerve cells in the prefrontal cortex. Those nerve cells may then increase their release of several emotion- and mood-regulating neurotransmitters, including dopamine, serotonin, and norepinephrine.
People who live with severe depression are thought to have an imbalance of the brain chemicals that regulate mood and emotion. Successful TMS therapy effectively increases the release of those brain chemicals, thereby restoring an appropriate balance and relieving depression symptoms.
For some people, just a single TMS session can increase neuron excitability (which is essential for neurotransmitter release). However, symptom relief typically doesn’t become noticeable until at least the third or fourth week of therapy.
TMS Therapy FAQ
Because transcranial magnetic stimulation is a relatively new depression treatment — it was approved by the FDA in 2008 — many people have questions about the safety and affordability of the therapy. Below, you’ll find answers to some of our most common queries.
Who Should Not Get TMS Therapy?
If you have any type of non-removable metal implanted in your head aside from dental fillings and braces, you should not get TMS treatments. The magnetic fields generated by the treatment coil can cause metal objects to malfunction, migrate, or heat up, all of which can cause serious complications or injury.
Are There Any Risks Associated With TMS?
Any type of psychiatric or medical treatment carries some degree of risk, and TMS is no exception. That said, side effects are typically mild and generally occur less frequently as patients acclimate to treatment.
The most common reported side effects are scalp discomfort and a headache after treatment, but not everyone experiences these issues. And although the risk is exceedingly low, and there are safety guidelines in place to minimize it, seizures have occurred. Compared to the side effects associated with antidepressant medications, however, TMS’s risks are remarkably mild.
Does Insurance Cover TMS Therapy?
Most insurance providers recognize TMS therapy as an essential form of healthcare and therefore provide coverage for treatments. However, most insurance companies also have strict requirements that must be met by the insured before coverage will kick in.
If you have questions about your eligibility for coverage, our Prime Behavioral Health team can help you determine whether you’ve met your insurance policy’s stipulations.
At Prime Behavioral Health in Southlake, we strive to provide exceptional psychiatric care and highly personalized treatment planning for each person who walks through our doors. If you or someone you love suffers from depression and may be able to benefit from TMS therapy, please don’t hesitate to reach out to our team for more information.
